Our user-friendly technology enables measurable outcomes for all our stakeholders.

At Medi Assist, we leverage our expertise and technology to provide top-notch health benefits administration services. Our seamless technology integration across the insurance and healthcare sectors has established us as a leader in high-quality service. Our custom-built, scalable, and secure infrastructure supports efficient, cost-effective operations. By investing in AI and data analytics, we anticipate trends, combat fraud, and enhance operations. Our user-friendly tools and streamlined checkouts improve the member experience, making insurance more accessible and convenient.
Here’s how we are leveraging technology to create an unparalleled ecosystem for our members, payors, providers and partners:
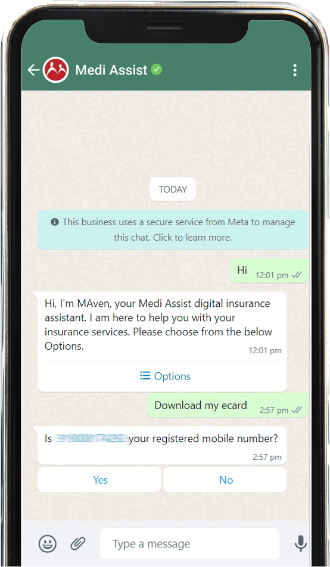
MAven Portal

MAven Portal
MAven Portal by Medi Assist is a web-based platform that allows members to manage their health benefits with the convenience of a desktop interface. It provides easy access to all policy details, including coverage and beneficiary information, simplifies policy terms, and allows for quick downloads of eCards. Users can find network hospitals, raise hospitalisation requests, submit reimbursement claims, and track claim statuses in real-time. The portal also supports managing dependents, accessing OPD benefits, and calculating out-of-pocket expenses (OOPE) for better financial planning. MAven Portal ensures that all your insurance needs are efficiently managed from one centralised location.
MAven App

MAven App
MAven App by Medi Assist is engineered to streamline health insurance management with exceptional ease. The app provides seamless access to comprehensive policy details, including coverage, inclusions, and beneficiary information. It simplifies the understanding of policy terms through clear underwriting information.
With the MAven App, users can swiftly download their eCard and those of their beneficiaries in under two minutes. The app features an efficient network hospital locator and allows for the convenient raising of hospitalisation requests and submission of reimbursement claims. Real-time claim tracking and instant notifications on claims and pre-authorisation requests are integral features, enhancing user experience.
Additionally, the app facilitates effortless management of dependents and supports OPD benefits. Users can calculate out-of-pocket expenses (OOPE) based on treatment details, aiding in financial planning and well-being. Overall, the MAven App consolidates all insurance needs into a single, user-friendly platform.
MAven Navigator

MAven Navigator
MAven Navigator is a pioneering capability developed by Medi Assist that predicts members' out-of-pocket expenses (OOPE). By using AI and ML the MAven Navigator provides an estimate based on the policy conditions, chosen treatment, room type, length of stay and hospital. MAven Navigator gives members a clear idea of their potential expenses. This valuable information enables members to make informed decisions about their hospitalisation.
MAven Claims
MAven Claims
MAven Claims is the cornerstone of Medi Assist, providing a comprehensive end-to-end platform designed to simplify the claims process for payers, customers, insurers and employees. The claims processing system streamlines our operations and provides a more objective and standardised approach to processing claims, allowing our processors to evaluate claims based on a structured set of guidelines. Instead of relying on subjective judgments, this approach empowers the processor to answer a few specific questions, enabling a consistent and efficient processing experience. MAven Claims reduces errors and delays. It streamlines the claims adjudication process and delivers exceptional service.
MAven Fraud Detection Engine (FDE)
MAven Fraud Detection Engine (FDE)
MAven FDE by Medi Assist is an advanced fraud detection engine designed to safeguard the integrity of health insurance claims. Leveraging sophisticated algorithms and data analytics techniques, MAven FDE automatically scrutinises large volumes of claims data to analyse patterns, trends, and outliers. By flagging potentially fraudulent claims for further investigation, it offers both speed and scalability in identifying suspicious activities. This powerful tool enables insurers to efficiently mitigate fraud risks across various claims, enhancing overall accuracy and operational efficiency. With MAven FDE, you can stay ahead and protect your organisation’s resources effectively.
MAven Insights
MAven Insights
MAven Insights is a cutting-edge data analytics function designed to transform how stakeholders leverage health claim data. In today’s competitive landscape, where data-driven decision-making is essential for growth, MAven Insights uses comprehensive claims data to deliver actionable insights that drive strategic decisions across health plans. The platform facilitates the identification, tracking, and visualisation of key business metrics, enhancing financial risk management and optimising care management as the industry shifts toward value-based care models. By ensuring reliable data, MAven Insights supports informed decision-making and helps mitigate risks.
At A Glance
At A Glance
The new 'At A Glance' page on our website brings real-time transparency into our SLAs and commitments to our healthcare ecosystem. It offers metrics on cashless services, reimbursements, and customer support, along with detailed data on new admissions and discharges. Users can track trends from daily to monthly and across different regions. Visit the ‘At a Glance’ page to experience how Medi Assist is leading the way in transforming visibility and transparency in healthcare.

Always by your side, making every experience easy and smooth
General helpline: 0120 693 7372
Senior citizen helpline: 1800 419 9493